How Trauma Affects the Brain — And What You Can Do to Heal
When Life Overwhelms You: Understanding Trauma in the Brain
Have you ever felt like your body just shuts down under stress? Or maybe you find yourself getting startled too easily, stuck in negative thoughts, or avoiding certain people, places, or memories? If so, you’re not alone. These can be signs that your brain has been deeply affected by trauma.
Whether it was one big event or a buildup of stressful experiences over time, trauma changes the way your brain works. But here’s the hopeful part: healing is absolutely possible. In this blog, we’ll break down what trauma does to your brain (in plain language!) and what you can do to feel more grounded, safe, and whole again.
What Happens in the Brain During Trauma?
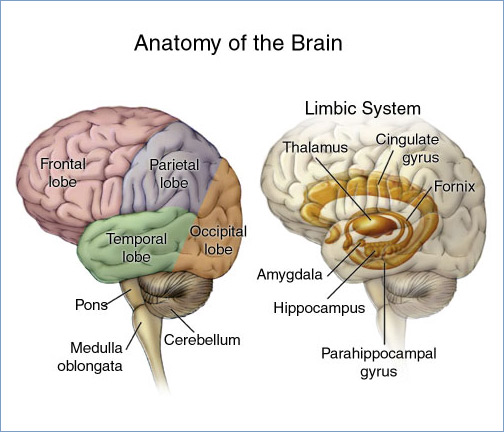
Our brains are made up of different parts that handle different jobs. When trauma hits, each part responds in its own way.
The Brain Stem: Fight, Flight, or Freeze
This is your survival brain—also known as the "reptilian brain." It's the part (medulla oblongata and pons) that jumps in when you sense danger. In trauma, this part can take over. You may freeze, collapse, lash out, or feel like you have to run away, even if there’s no actual danger right now. You might notice fast breathing, racing heart, or tight muscles.
The Limbic System (Midbrain): Where Emotions Live
This part of your brain handles emotions and memories. The hippocampus and amygdala are here. These areas get overworked during trauma, and that changes how you store and recall memories.
Hippocampus: Helps sort past from present. But after trauma, it can shrink—making it hard to feel like the bad thing is really over.
Amygdala: Tags memories with emotions like fear or sadness. Trauma can make this part super alert, causing you to feel constantly on edge or fearful.
The Cortex (Forebrain): Thinking and Decision-Making
This is the “thinking brain.” It helps with focus, planning, and calming down. After trauma, it may not work as well:
Prefrontal Cortex: Shrinks and becomes less flexible. This can make your thinking feel rigid or stuck.
Orbitofrontal Cortex: Can become more active—meaning you may stay overly alert or "hyperaware" of your surroundings.
Signs Your Brain Is Still Reacting to Trauma
After trauma, your brain can stay in a kind of "emergency mode" long after the event has passed. Here are some common experiences:
Intrusive thoughts: Unwanted memories or flashbacks
Mood swings: Sadness, shame, or feeling numb
Hypervigilance: Feeling constantly unsafe or "on guard"
Avoidance: Avoiding anything that reminds you of what happened
What Science Shows: Dr. Amen’s Brain Scans
Dr. Daniel Amen has done brain scans (called SPECT scans) on people who’ve experienced trauma. Many show a “diamond pattern,” with overactive regions like:
Anterior cingulate gyrus: Makes it hard to shift thoughts—leading to rumination or obsession.
Basal ganglia & amygdala: Heightens anxiety and fear responses.
Thalamus: Boosts sensitivity to sights, sounds, and feelings.
Right lateral temporal lobe: Can cause you to misread social cues or see threat where there isn’t any.
All of this explains why even small things might feel big after trauma. Your brain is working overtime to keep you safe.
You Can Heal: Steps Toward a Calmer, Safer You
The good news? You’re not stuck. Your brain is changeable, and healing is possible. Here are steps that can really help:
1. Try Trauma-Informed Therapy
Working with a therapist trained in trauma can be life-changing. Therapies like:
EMDR (Eye Movement Desensitization and Reprocessing)
CBT (Cognitive Behavioral Therapy)
DBT (Dialectical Behavior Therapy)
Mindfulness-Based Therapy
These can help your brain make new, healthier connections.
2. Practice Body-Based Healing
Trauma lives in the body too. Try:
Yoga or stretching
Deep breathing exercises
Progressive muscle relaxation
These can calm the nervous system and bring your brain out of "emergency mode."
3. Build a Support Network
Healing is hard alone. Stay connected with safe friends, support groups, or family. Social connection helps the brain rebuild trust and safety.
4. Write It Out
Journaling helps process and organize thoughts and emotions. It also supports brain regions responsible for memory and regulation.
5. Move Your Body
Regular exercise increases brain chemicals like dopamine and serotonin, which improve mood and brain function.
6. Pay Attention to Nutrition and Supplements
Certain vitamins (like Omega-3s and B-complex) support brain health. Sometimes a dose of oxytocin helps. Talk to a healthcare provider about what’s right for you.
Final Thoughts: Your Brain Can Heal
You are not broken. The symptoms you're experiencing are not character flaws—they are your brain doing its best to survive. And now that you're safe enough to notice them, it's a sign that healing can begin.
Whether through trauma therapy, movement, writing, or connection, your brain can learn that it’s okay to let go of that constant state of alertness. It takes time—but with the right support, it’s absolutely possible.
Ready to Start Healing?
If you’re wondering how trauma may be affecting your brain—or if you're ready to take the next step in your healing journey—I’d love to talk. I offer free 15-minute phone consultations to help you explore if trauma therapy in Denver, CO is right for you.
👉 Click here to schedule your free consultation or call 720-577-5571.
Let’s help your brain and body feel safe again—together.
FAQ: How Trauma Affects the Brain
1. Can trauma really change my brain physically?
Yes. Trauma can shrink or overstimulate certain areas of the brain, especially those tied to memory, emotion, and thinking.
2. What are the most common signs that trauma has affected my brain?
Trouble sleeping, being easily startled, mood swings, flashbacks, and avoidance are all common.
3. Can therapy reverse these changes?
Trauma therapy can help “rewire” the brain. With time and the right support, many people experience major improvements.
4. What’s the best kind of therapy for trauma?
EMDR, CBT, DBT, and mindfulness-based therapies are often effective.